The relevance of studying the development mechanism of chronic prostatitis increases in proportion to the increase in the number of diagnosed cases of the disease. It is known that chronic prostatitis (CP) occupies a leading position among urinary pathologies and is the result of many factors that are an integral part of modern life (social environment, biology, etc. )state, an increase in the resistance of pathogens to antibacterial drugs).
Since the disease not only includes an increasing percentage of the male population, but is also diagnosed at an increasingly younger age, doctors often have a dismissive attitude towards it, those who use a model regimen for treatment that is unlikely to lead to recovery.
What is chronic prostatitis?
The diagnosis of chronic prostatitis (CP) combines a series of pathological processes in the prostate gland, which manifest as a chronic inflammatory process of tissues. However, one cannot refer only to CP due to pathogen penetration into the prostate, since such a view justifies efforts to treat prostatitis with antibiotics alone, almost nevernow brings positive long-term results.
The main factors underlying the development of pathology can be considered as complex changes in the tissues and, therefore, the functional capabilities of the gland, which are the main causes of the development of the microflora. infectious birth. Chronic prostatitis is, to a certain extent, a general diagnosis that combines several factors:
- Reduced immunity.
- Process stagnation in the pelvic organs.
- Urinary disorders.
- Degenerative process in prostate parenchyma.
- Nutritional disorders.
- inflammatory processes.
Development Mechanism
The penetration of pathogenic microflora into a healthy prostate gland is practically impossible to provoke an inflammatory process, since the microflora of the prostate has a certain resistance to pathogens present in the urethra. However, the presence of one or more of the above triggers leads to the development of persistent inflammation, accompanied by the appearance of scar formation (fiberization) or areas of necrosis.
The proliferation of connective tissues during scar formation causes congestion in the acini (the duct that ensures the secretion of secretions), exacerbating the course of the disease. Necrosis of tissues leads to the formation of a cavernous body, in which, in addition to the dead epithelium, a prostate secretion is deposited.
Thus, the main cause of the development of CP is not infection, but various physiological disorders that allow the inflammatory process to become chronic.
Another distinguishing feature of the disease, which makes diagnosis difficult, iscyclicity of the flow. As a rule, under the influence of external factors or the internal state of the body, there is a cyclical change in the intensity of the pathology, during which acute conditions are replaced by periods. remission.
There is often not only the complete absence of symptoms, but also the absence of laboratory indicators for the presence of infection (eg, white blood cells). Despite the positive results, the condition cannot be considered as a recovery, since all physiological disturbances in the gland remain unchanged.
The reasons
The main causes of circulatory disorders in the pelvic organs and stagnation of venous blood in the prostate are:
- Stay permanently in a sitting position.
- Hypothermia in the whole body or directly in the pelvis.
- Whole body constipation.
- Abstain from prolonged sexual activity or excessive sexual activity.
- The presence in the body of a chronic infection of any locality (sinusitis, bronchitis).
- Excessive physical activity, accompanied by lack of sleep or rest, will cause immunosuppression.
- History of urogenital infection (gonorrhea, trichomoniasis).
- Toxic effects on the body due to the systematic use of alcoholic beverages.
The presence of any of these causes leads to the appearance of stagnant processes, a decrease in the secretory function of the glands, a decrease in cellular resistance to diseases, contributes to theoptimal conditions for the reproduction of pathogenic microorganisms in the prostate gland. .
Can chronic prostatitis be cured?
Although there is a large amount of systematized information on the CP development mechanism,Its treatment is extremely difficultand is one of the leading problems in modern urological practice.
Due to the fact that the disease progresses in each patient according to an individual scheme, therefore, the therapeutic approach must also be individual, taking into account all the physiological changes that have occurred in the prostate gland.
The anatomical features of the prostate gland, which can be accessed through the urethra or rectum, significantly reduce the effectiveness of the applied therapeutic effect. In this regard, in order to achieve a relatively stable result, a long course of treatment (usually several months) is required, during which the patient must strictly follow all the instructions of the doctor.

Unfortunately, it can only be completely curedin 30 cases over 100. This is mainly due to the lack of prompt medical help, the long absence of severe symptoms, or the conscious avoidance of uncomfortable diagnostic and subsequent treatment procedures. As a rule, at the time of treatment, the process of atrophy of the prostate gland is irreversible, and even with long-term treatment, only complete elimination of symptoms and stable remission, duration, is possible. depends on patient compliance. with the doctor's recommendations.
The treatment
The complex of measures used in the treatment of CP includes:
Antibacterial therapy
The inhibition of the activity of the microflora with the help of antibiotics should be carried out only after a series of laboratory tests, according to the results of the most effective drug prescribed.
As a rule, the duration of antibiotics is determined by the severity of the disease and is at least 30 days. Interruption of treatment is unacceptable, as the remaining microorganisms will become resistant to this class of drugs, and then they will need to be replaced and even longer. In the treatment of prostatitis, priority is given to the use of antibiotics with bactericidal effect:
- Fluoroquinolones;
- Azalides;
- Aminoglycosides;
- Tetracyclines.

If laboratory tests reveal a specific nature of the infection, for example, trichomoniasis or a viral origin of prostatitis, nitroimidazoles or antivirals are prescribed in parallel with antibiotics. .
The use of antispasmodics and α . blockers
The main purpose of using drugs of this class is to reduce spasms in the pelvic floor, help increase blood supply, improve urine output, and relieve pain.
Laxative
To avoid undue strain on the pelvic muscles that occurs during defecation, laxatives should be used, since attempts at constipation may aggravate the patient's condition.
Physical therapy
One of the popular physical therapy methods is prostate rectal massage. Therapeutic effects of fingering on the prostate gland, performed through the anus, to force the infected secretions out, which is then excreted through the urethra.
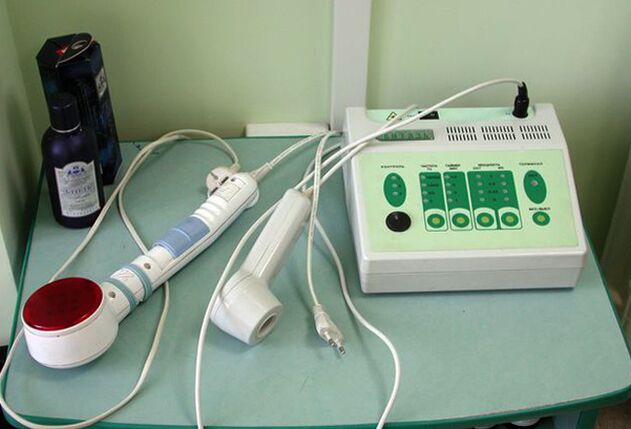
In addition, during massage, the blood supply to the tissues increases, which has a positive effect on antibiotic therapy. To perform rectal prostatic massage, the following physiotherapeutic methods are also used:
- Electrical simulation.
- High frequency heat therapy.
- Infrared laser therapy.
Prevent
Once the condition stabilizes, the patient is asked to follow rules that impose some restrictions on the usual lifestyle:
- Avoid processes that use water in open reservoirs and pools.
- Regularly visit your doctor.
- Absolutely no alcohol.
- Have a regular sex life with a partner.
Compliance with the rules will allow you to go into remission as long as possible and avoid exacerbations of the disease.































